
Experts agree: There is no such thing as “Super Flu”.
KIT KNIGHTLY
Currently, the headlines all across the United Kingdom, and a handful of other nations, are full of references to “Super Flu”.
There is no such thing as “Super Flu”.
It is a term with no scientific meaning or even a solid definition. To confirm this we need look no further than this report from Channel 4 News:
NHS England is calling it a ‘super flu’, which is in fact its own phrase rather than anything scientific.
Or, even more tellingly, there is Devi Shridhar — the High Priestess of Covid hysteria herself — whose Guardian column is headlined “Don’t Call it the Super Flu”, and begins:
I should start by saying “super flu” is not a scientific term or one used by any academics or clinicians I work with. It’s a colloquial phrase that’s been used by various NHS England bosses and taken up by Wes Streeting, the health secretary, and Keir Starmer.
That’s that then. The experts have spoken: “Super Flu” is a colloquial phrase with no actual meaning.
So why does everyone keep describing the incipient flu season in those terms?
To quote Shridar again:
Amid all the noise, it’s difficult to know how bad this flu really is – and how much is political spin.
Isn’t it just?
Maybe it’s time we found out how bad this flu really is, and what about it (if anything) is “super”.
First, we should ask: Doe this flu have different symptoms? Or are the symptoms more severe?
It doesn’t, and they are not, as Dr Giuseppe Aragona tells the Independent [emphasis added]:
The symptoms and severity of H3N2 illness have been similar to seasonal flu, including fever, cough, runny nose, and possibly other symptoms, such as body aches, vomiting, or diarrhoea.
Ok, so its symptoms are common and not unusually severe. Then maybe it’s more transmissible? Or deadly?
Nope. At least, not according to the WHO experts quoted in Politico [emphasis added]:
While hospital admissions have been rising sharply due to the early arrival of flu season, there is currently no evidence that this season’s variant is more deadly or transmissible, experts at the World Health Organization (WHO) and the European Centre for Disease Prevention and Control (ECDC) told POLITICO.
OK, let’s sum up what we know so far:
- This flu has no unusual symptoms.
- Its symptoms are not unusually severe.
- It is not any more transmissible than normal.
- It is no more deadly than normal.
It seems there is nothing even odd about this flu, let alone “super”.
A lot of the news coverage is focusing on the potential danger to the NHS, with headlines warning this is “beyond catastrophic” and “pushing the NHS to the brink”.
But anyone with a half-decent memory, or the ability to Google, will tell you that headlines warning of overcrowded hospitals or a “winter crisis” are a yearly tradition in the UK:
The BBC explainer Flu in five charts – how this year’s winter outbreak is different even quotes experts who point this out, and notes that the NHS isn’t close to breaking point [emphasis added]:
Health experts at the King’s Fund think tank have said talk of an “unrelenting flu wave” has become worryingly familiar over recent years. But Chris Streather, the medical director for the NHS in London, said the situation was “well within the boundaries” of what the NHS could cope with.
So, it’s not an unusual flu, the NHS is not unusually strained, and there’s no overcrowding at all (so far).
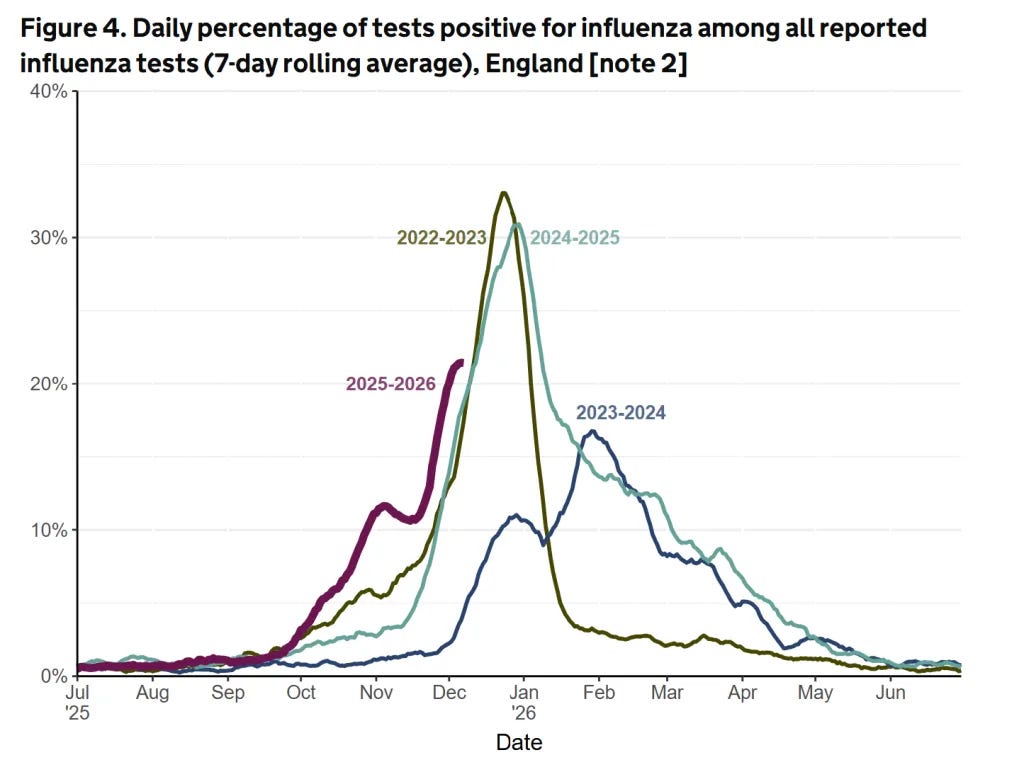
The only aspect that seems even vaguely out of the ordinary is the timing. The BBC’s first graph displays this:
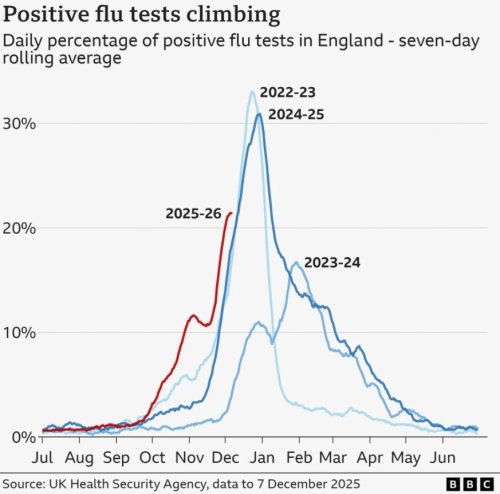
Looking at this graph (supposing it’s based on actual data) you can see the flu season spike starts roughly a week earlier than recent years. Some outlets are calling this unprecedented, but they are only comparing it to the last three or four years, so we have no idea if that’s true. The rate of increase is inline with the past, and it appears to be peaking already.
The government figures show the number of people visiting their GPs with “influenza-like illness” is basically normal, if again spiking slightly earlier than average:
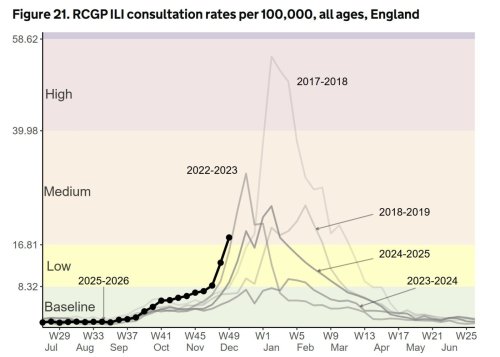
A little search engine research will get you similar figures going back to 1999/2000, all spiking in-and-around week 49.
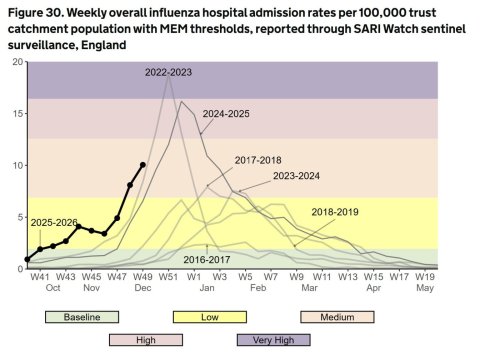
Likewise, the number of people being admitted to the hospital for flu is normal for the time of year:
Let us summarize one last time. The super flu:
- Has common symptoms.
- Of regular severity.
- It isn’t unusually infectious.
- Or especially deadly.
- The NHS isn’t more crowded than normal
- And is well within thresholds.
- A normal number of people are going to the GP.
- Resulting in a predictable rate of hospitalization.
Hardly “super”, is it?
None of this is “conspiracy theorist” stuff either, it is all mainstream data. These are the “experts” we’re supposed to listen to and the “science” we’re encouraged to follow.
And yet we’re faced with this bizarre situation, where the news in general is telling everyone to be scared, while the specifics go out of their way to highlight the fact there is, as yet, nothing at all to be scared of.
It all feels oddly familiar, doesn’t it?
This article (Experts agree: There is no such thing as “Super Flu”) was created and published by off-Guardian and is republished here under “Fair Use” with attribution to the author Kit Knightly
See Related Article Below
SuperFlu is Flagellistic (expialidotious)
The Sound Is Quite Atrocious, the Data Are Not
HART
Once again, as Christmas approaches, we are told the NHS is on the brink. Headlines warn of a “superflu” season threatening to overwhelm hospitals, with language that feels uncomfortably familiar. The sense of déjà vu is striking. In 2020, the public was told that extraordinary interventions were justified because the situation was exceptional. There is nothing exceptional about the current circumstances, yet across Europe the same crisis framing has returned.
Despite the absence of evidence for anything exceptional, there is a strong sense of Déjà vu. In the UK, schools have begun closing pre-emptively, particularly in Wales – some describing this as a “firebreak” as if transmission can be controlled by wiping surfaces. In Leeds, with Christmas on the horizon, children have been banned from singing in assembly. Vaccination messaging has intensified too. Flu vaccines are being pushed beyond traditional risk groups, including toddlers, once again framed as a moral duty, to “protect granny”.
What does the data show to justify this? The overall hospital admission rates are broadly in line with recent years, merely shifted earlier by perhaps a week or two. The WHO admitted the earlier start way back in November.

Test positivity for influenza has begun to slow over recent days suggesting an approaching first peak for the season.
Part of the problem is the use of a model to estimate the amount of flu at any one particular time of year. This model is only comparing current levels with levels that day or week in previous years. It is incapable of noticing that the same trajectory has simply moved to be earlier.
Whether there is a second peak later in the winter remains to be seen, but this is not in itself a cause for alarm. Multiple peaks are a familiar feature of some flu seasons. Across hospital admissions, test positivity and primary-care surveillance, current levels remain well below those seen during more severe recent winters, including 2022–23 after accounting for an earlier start.
Perspective matters. NHS England recently reported around 2,600 patients in hospital with flu. Spread across more than 1,000 hospitals, this equates to an average of roughly three patients per hospital. Any additional pressure on an already stretched system matters, especially with uneven distribution of cases – but this is a long way from an unprecedented national emergency.
We are told influenza travels with world peaking in Australia during our summer and in the northern hemisphere during their summer. We are told that influenza vaccines can be modelled on the Australian variants for use in the northern hemisphere. This year the Australia flu peak was less high and the overall wave was more spread out.

More testing, more “cases”
One factor almost entirely absent from media reporting is the impact of surveillance itself.
We now test for respiratory viruses at a scale and intensity that would have been unthinkable before 2020. Multiplex PCR panels are widely used in hospitals. Sentinel GP surveillance has expanded. Schools, care settings and hospitals are all more likely to test, earlier and more often.
Much of what is being labelled “record flu” is therefore better understood as record detection, not record disease. Increased testing inflates case counts, shifts thresholds and makes comparisons with earlier years unreliable unless surveillance intensity is properly accounted for. Also, the monitoring systems have alerts when rates are high for the day or week of the year with no accounting for an earlier season.
The illogical position on masking
There is a deeper inconsistency at the heart of current messaging.
During Covid, the public was repeatedly told that SARS-CoV-2 was fundamentally different from influenza, and that extraordinary measures were justified precisely because it was not like flu. That claim underpinned lockdowns, mask mandates and school closures.
That logic has now quietly flipped.
Across Europe, people are once again being encouraged to adopt population-wide interventions – including masking – in response to a virus that is flu: a seasonal pathogen that returns every winter and always will.
This matters because the evidence showed masking did not work for preventing respiratory viruses. The evidence based that is used to support masking relies on either models that assume masks work then conclude they work well, or on laboratory studies that attempt to collect virus projected forwards but ignore the fact air is redirected to the sides with masking. The best-quality evidence, including real-world natural experiments such as medical-grade mask mandates in Austria and Germany, failed to demonstrate meaningful benefit during covid and there is no reason to expect different results for other aerosolised respiratory viruses. Wes Streeting is failing to lead on this saying he will not issue country wide mandates because of this lack of evidence yet “supports” NHS leaders who want to issue them locally.
Re-deploying the same interventions year after year for endemic seasonal viruses risks normalising emergency measures without ever demonstrating that they meaningfully work. Masks are not a benign intervention. They strip humans of the emotional connections made with smiles and our ability to assess danger such that every stranger becomes someone to be cautious of. They measurably affected language development in children who need to see mouths when in their finite window of language development. They hamper communication with devastating effects for deaf people and create real risks in healthcare settings where clear communication can be a matter of life and death.
Flu does not warrant covid-era responses and covid was also never exceptional in the way the public was told.
Vaccination
Uptake of flu vaccination among children has risen sharply in recent years, particularly following expansion into secondary school age groups. It is children this age who have the highest positivity rates for flu.
There is an additional and largely unexamined issue. As with Covid vaccines, trials of children’s nasal flu vaccines typically ignore what happens in the first two weeks after administration. Any primary school head teacher can attest that these campaigns are often followed by widespread illness in the immediate aftermath, yet this observation has not been examined systematically. The obvious questions are never asked. Are these vaccines simply bringing infections forward? Was the earlier vaccination campaign itself a contributor to this year’s earlier surge?
These are not fringe concerns. They are questions of critical importance and their consistent absence from official discussion is itself revealing.
Conclusion
There is no “super-flu” just the usual flu trajectory happening a week or two earlier. The response has been close to hysterical but is revealing in terms of its lack of logic, evidence base and lessons learned since 2020. A striking feature of the current moment is not the epidemiology, but the synchronisation of alarm across Europe. Within the same weeks, multiple countries have issued near-identical warnings of hospitals being “on the brink”, invoked exceptional seasonal pressure from influenza, and floated or re-introduced non-pharmaceutical interventions such as masking in healthcare settings.
Public health depends on credibility. When every winter is framed as unprecedented, and every seasonal virus as an emergency, the result will be a drop in trust. Enough damage has been done. This must stop.
STOP PRESS: Smile Free and Together Declaration have joined forces with a campaign tool to write to Wes Streeting and Dame Jenny Harries to stop further calls for masks. Link here.
This article (SuperFlu is Flagellistic (expialidotious)) was created and published by Hart and is republished here under “Fair Use”






Leave a Reply